Past Issues
Prevalence of Gastroduodenal Disease with Helicobacter Pylori in the Region of Tiaret, Algeria
Souhila Tabak1*, Mohamed Djamel Miara1, Hamdi Bendif2, Luca A. Vitali3
1Department of Nature and Life Sciences, University of Ibn Khadoun, Tiaret, Algeria
2Department of Natural and Life Sciences, Faculty of Science, University of M'sila, M'sila, Algeria
3School of Pharmacy, Microbiology Unit, University of Camerino, Camerino (MC), Italy
*Corresponding author: Souhila Tabak, Department of Nature and Life Sciences, University of Ibn Khadoun, Tiaret, Algeria. Tel: 213778678682 Email: [email protected]
Citation: Tabak S, et al. (2022). Prevalence of gastroduodenal disease with Helicobacter pylori in the region of Tiaret, Algeria. Traditional Medicine. 3(2):12.
Received: May 27, 2022
Published: Oct 21, 2022
Copyright: Tabak S, et al. © (2022).
ABSTRACT
The objective of this work is to carry out a retrospective epidemiological study of Helicobacter pylori infection in the region of Tiaret, Algeria.We have carried out a retrospective study of Helicobacter pylori infection in patients with gastroduodenal diseases, consulting a gastroenterologist in the region of Tiaret. The rate of H. pylori infection is 43.71%. Similarly, we observed a significant increase in the rate of H. pylori infection with age, with a peak rate of (24.66%) occurring in the 30-40 age group. This rate is significantly related to age, and gender had no effect on the prevalence of infection, which is mainly associated with gastritis (82.19%).
Keywords: Retrospective study, Helicobacter pylori, Gastritis
INTRODUCTION
The discovery of H. pylori in 1982 revolutionized the understanding of pathophysiology and the management of gastroduodenal disease and as such represents one of the most significant recent advances in microbiology [19].
H. pylori is found mainly in the stomach, both in the antrum and in the funds, and can be isolated from gastric fluid under normal acid conditions [22].
The highest prevalence is observed in developing countries such as Latin America and Africa, which appears as an index of socioeconomic level [21].
H. pylori infection is probably the most common infection worldwide and is estimated to affect about 40% of the world population and 20-90% of adult individuals are infected depending on the country, with infection being more common in disadvantaged, low socioeconomic settings (Joutei et al., 2010).
The prevalence observed today is the consequence of socioeconomic conditions and the environment [20].
According to a scientific study, H. pylori, a bacteria living in the gastric environment, affects more than 90% of the Algerian population [30]. Gastroenterology specialists are sounding the alarm bells because they believe this disease could become the disease of the century [16].
Our work is carried out within the framework of a prevalence of H. pylori-related gastroduodenal diseases in the Tiaret region of Algeria.
METHODS
Study population
In this study, the objective was to assess the prevalence of gastroduodenal disease with H. pylori, 260 patients consulting gastroenterologists in the Tiaret region, and to study their distribution according to implication or not of H . pylori in the disease, sex, age groups, and type of pathology related to this bacterium.
Type of study
This is a retrospective epidemiological study involving 260 patients with gastroduodenal disease (110 men and 146 women), ranging in age from 12 to 82 years. The study took place in Tiaret, from November 2014 to April 2015, and was conducted in gastroenterology practices.
Inclusion criteria
Our study is about the Patient:
- From the Tiaret region, Algeria
- Suffering from gastroduodenal diseases with H. pylori or not;
- Underwent a gastric biopsy
Statistical Analysis
Descriptive statistics, counts, and percentages were calculated using IBM SPSS Statistics Subscription Trial for Microsoft Windows 64-bit. IBM SPSS non-parametric one-sample Chi-square test (p ≤ 0.01).
RESULTS
Involvement of H. pylori in gastroduodenal diseases
Among the 260 patients suffering from gastroduodenal diseases, we found 152 patients infected with H. pylori, giving an infection rate of 58.46%. The results are shown in the following histogram.
HP+: Infected with H.pylori
(χ2 = 6.24. p ≤ 0.01).
HP+: Infected with H.pylori
HP-: Not infected with H.pylori
Figure1. Percentage of patients infected or not with Helicobacter pylori
Distribution of H. pylori infection by gender
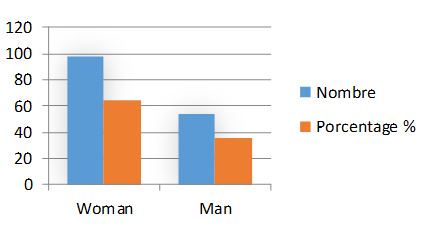
The incidence of H. pylori infection was slightly higher in females (64.47%) compared to males (35.53 %). However, this difference was not significant. The results of this study indicate that gender had no significant effect on the prevalence of H. pylori infection. Fig 2.
(χ2 = 8.57. p ≤ 0.01)
Figure 2. Distribution of Helicobacter pylori infection by sex of patients
Distribution of H. pylori infection by age group
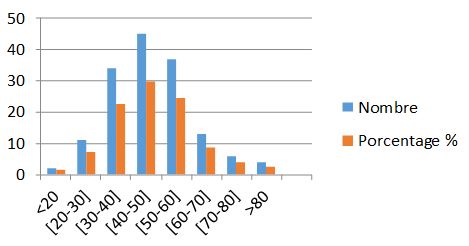
We observed a significant increase in the prevalence of H. pylori infection with age, with a peak rate (29.60%) occurring in the 40-50 age group. The results can be represented by a graph (Fig. 3) to make the results clearer and more readable.
(χ2 = 9083. p ≤ 0.01)
Figure 3. Distribution of H. pylori infection according to patient age groups
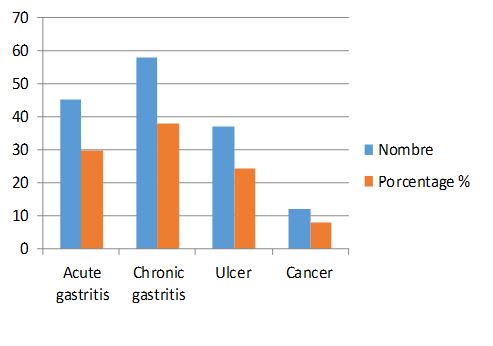
Distribution of H. pylori infection according to type of pathology
These patients all present with gastric disorders at different levels of the stomach. Among 152 patients infected with H. pylori, (29.6%) of patients had acute gastritis, (38.15%) of patients developed chronic gastritis, (24.34%) of patients had an ulcer, and (7.89%) of patients suffering from cancer. To shed light on these results we have represented them in the form of a graphical area (Fig. 4).
(χ2 = 23.68. p ≤ 0.01)
Figure 4. Distribution of patients infected with H. pylori according to type of gastric pathology
DISCUSSION
The prevalence of H. pylori infection is between 20 and 40% in industrialized countries; it reaches 70 to 90% in developing countries [19]. Whereas in our study population, the prevalence rate is 58.46%, which corresponds more or less to half of the prevalence found in Algeria (78%).
H. pylori infection is higher in developing countries (78% in Algeria, 71% in Morocco, 69% in Côte d'Ivoire) [11].
Elmanama et al., [8] demonstrated that both sexes are equally affected by H. pylori infection, confirming the results of our series. However, other studies have noted a male predominance [21].
Furthermore, if we compare by age group, H. pylori are found in our series at a rate of 29.60% in patients between 40 and 50 years of age. This average is lower than the European figures, which are around 60 years [13], whereas, in other studies of Everhart, 2000, no significant difference has been reported for age groups, some studies have shown that contamination occurs early in childhood, and before the age of 10 years, more than 50% [15].
Ilboudo et al., [17] argue that in Africa, every individual taken in adulthood and whatever his socio-economic level has lived a childhood in an environment conducive to contamination because H. pylori is responsible for the development of several gastric pathologies. It is responsible for 80% of chronic atrophic gastritis [22]. As a result of the inflammatory and immunological response induced by this bacterium, 1 to 10% of peptic ulcers and 1 to 3% of gastric cancers result from it [3]. These results are consistent with those found in our study. Indeed, H. pylori are most often linked to gastritis with a rate of 67.75%. As well, the frequency of peptic ulcers in the population infected with H. pylori was 24.34% and it was 7.89% in the case of cancer.
Moroccan authors presume that H. pylori are indeed correlated most often with chronic atrophic gastritis with a prevalence of 95.56% [1]. It is now clearly established that H. pylori are responsible for gastric cancer and that no such cancer develops in the absence of this bacterium [6]. Nevertheless, the number of patients at risk of developing cancer is small compared to the size of the population infected with H. pylori [26], this is consistent with the results of our series where 7.89% of our population had developed cancer.
CONCLUSION
This study shows the very high prevalence of patients suffering from gastroduodenal diseases in the region of Tiaret, which reveals incriminating Helicobacter pylori. These results also show that age, sex, and pathology are factors playing an important role in the prevalence.
CONFLICTS OF INTEREST
The author declares they have no conflicts of interest.
FUNDING
The author received no financial support for this research.
ACKNOWLEDGMENTS
The authors would like to sincerely thank the personnel of Hospital Center Youssef Damedji–Tiaret, Algeria for their contribution to this study. Special thanks to Dr. Belarbi Mohamed gastroenterologist for his help.
REFERENCES
1. N. Attaf, N. Cherkaoui, M.K. Choulli, L. Ghazali, A. Mokhtari, A. Soulaymani. (2004). Profil épidémiologique de l’infection à Helicobacter pylori dans la région du GharbChrarda-Beni Hssen. Biologie & Santé. 4(1):25- 34.
2. Binan Y, Adom H, Tanon A, Toutou T, Yao H. (2006). Cancer gastrique et Helicobacter pylori: résultats d’un centre d’endoscopie à Abidjan. Revue Internationale des Sciences Médicales. 8(1): 23–27.
3. Brown. L.M. (2000). Helicobacter pylori: epidemiology and routes of transmission. Epidemiol Rev. 22(2): 283-297.
4. Corallo J. (1991). Helicobacter pylori. Acta Endoscopica. 21(1):112–117.
5. De Giacomo C. (1994). Transmission de l’infection à Helicobacter pylori,chez l’enfant. La lettre de l’infectiologue. 4 (suppl), IX : 8–9.
6. Delchier. JC. (2003). Le lymphome gastrique du MALT, une infection maligne potentiellement curable par l‘éradication de Helicobacter pylori. Gastroentérologie Clinique et Biologique. 27(3) :453–458.
7. Diomande MI. (1991). Gastrite chronique et infection à Helicobacter pylori en Côte d’Ivoire : étude d’une série de 277 patients symptomatiques. Gastroentérologie Clinique et Biologique. 15(10) : 711–716.
8. Elmanama A, Mokhallalati M, Abu-Mugesieb R, Abdelraouf, Mahmoud R. (2008). Risk factors 10. associated with Helicobacter pylori infection in Gaza, Palestine. The Islamic University Journal. 16(2): 97–110.
9. Essadik A, Benomar H, Rafik I, Hamza M, Guemouri L, Kettani A, et al. (2013). Aspects épidémiologiques et cliniques de l’infection à Helicobacter pylori à travers une étude marocaine. Hegel. 3(3) :163-169.
10. Everhart JE. (2000). Recent developments in the epidemiology of Helicobacter pylori. Gastroenterol Clin North Am. 29 (3): 559-578.
11. Faik M. (2000). Mise au point sur l’infestation gastrique par Helicobacter pylori. Médecine du Magreb. N. 79,2000. Pp (17-19).
12. Fukushima T, Strauss RM, Waring JP. (2000). Male predominance of H. pylori associated hypertrophic gastritis is explained by tobacco and alcohol use: an evidence for host-mediated inflammatory response to H. pylori gastritis. American Journal of Gastroenterology. 95(9) :2452-2452.
13. Jouti H, Hilali A, Fechtali T, Rhallabi N, Benamair H. (2010). L’infection à Helicobacter pylori chez 755 patients présentant des symptômes digestifs institut pasteur du Maroc, 1998-2007. Eastern Mediterranean Health Journal; Alexandria. 16(7) : 778-782.
14. Harrics AD. (1992). Helicobacter pylori in Malawi, central Africa. Journal of Infection. 24 : 265–276.
15. Haruma K. (2000). Trend toward a reduced prevalence of 22. Helicobacter pylori infection, chronic gastritis, and gastric cancer in Japan. Gastroenterol Clin North Am. 29(3): 623-631.
16. Houria K, Koula D, Ahmed A, Souhila T, Hasna B. (2019). Epidemiological Profile of Helicobacter pylori Infection in Patients with Digestive Symptoms in Algeria. J Epidemiol Glob Health. 10(4):293-297.
17. Bougouma A, Diomande I, Ilboudo, Sangare L, Sanou J. (1997). Aspects épidémiologiques et cliniques de l’infection à Helicobacter pylori en zone tropicale : à propos de 150 patients à l’hôpital national de Ouagadougou (Burkina Faso). Med. Afr. noire (En ligne). 44 (1) : 24-28.
18. Glupczynski Y. (1994). Epidémiologie de l’infection à Helicobacter pylori et méthodes diagnostiques. Annales Médicales de Nancy et de l’Est. 339(2) : 89–93.
19. Glupczynski Y. (2000). Helicobacter pylori : actualité dans les domaines du diagnostic de la clinique et du traitement. Arch public Health. 58 : 145-153.
20. Magalhaes DM, Luzza F. (2006). Epidemiology of Helicobacter pylori infection. Helicobacter. 11(1):1–5.
21. Malaty HM. (2007). Epidemiology of Helicobacter pylori infection. Best practice and research clinical. Gastroenterology. 21(2): 205-214.
22. Marshall BJ, Warren JR. (1984). Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 323 (8390) : P1311-1315.
23. Mignon M. (2005). Prix Nobel de Médecine 2005 : Barry J. Marshall 1.et J. Robin Warren. Helicobacter pylori couronné. Médecine Sciences. 21(11) : 993–994.
24. Rafeey M, Nikvash S. (2007). Detection of Helicobacter pylori antigen in stool samples for diagnosis of infection in children. East Mediterr Health J. 13(5):1067–1072.
25. Ramanampamonjy RM, Randria MJD, Razafimahefa SH, Ratsimandisa R, Rajaonarivelo P. (2007). Séroprévalence de l’infection due à Helicobacter pylori dans un échantillon de population malgache. Bull Soc Pathol Exot. 100(1) : 57- 60.
26. Schistosomes, liver flukes and Helicobacter pylori. (1994). IARC Monogr Eval Carcinog Risks Hum. 61:1–241.
27. Seoane A, Bessa X, Balleste B, O'Callagha. E, Panadès A, Alameda F. (2005). Helicobacter pylori and gastric cancer: relationship with histological subtype and tumor location. Gastroenterol Hepatol. 28(2): 60-64.
28. Sobala GM, Crabtree JE, Pentith JA, Rathbone BJ, Shallcross TM, Wyatt JI. (1991). Screening dyspepsia by serology to Helicobacter pylori. Lancet. 338(8759): 94–96.
29. Thomson AB, Chiba N. (1998). From bench to bedside and back- 2. report on the European Helicobacter pylori Study Group Xth International Workshop on Gastroduodenal Pathology and Helicobacter pylori. Can J Gastroenterol. 12(6): 437–446.
30. Vincent. P. (1995). L’abitat d’H-pylori et sa desimanationdan la population donnees récentes Hepato Gastro n°2 (uppl 1). 2: 7-16.
Copyright: Tabak S, et al. © (2022). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
 Abstract
Abstract  PDF
PDF.JPG)